Chronic lameness in Akita Inu, two years after TTA
Corresponding author:
Dr. Vladislav Zlatinov,
Central Veterinary Clinic-Sofia, Bulgaria
Eri is a three years old male Akita Inu dog, weighing 39 kg. The dog was presented because of left hind leg lameness, lasting for about 4 months. A surgical treatment-Tibial Tuberosity Advancement (TTA) for cranial cruciate insufficiency had been done at the same leg, about 2 years ago. Eri is a pet dog, but has an active lifestyle- long walks (>8 kms) covered regularly.
History
Previous treatments
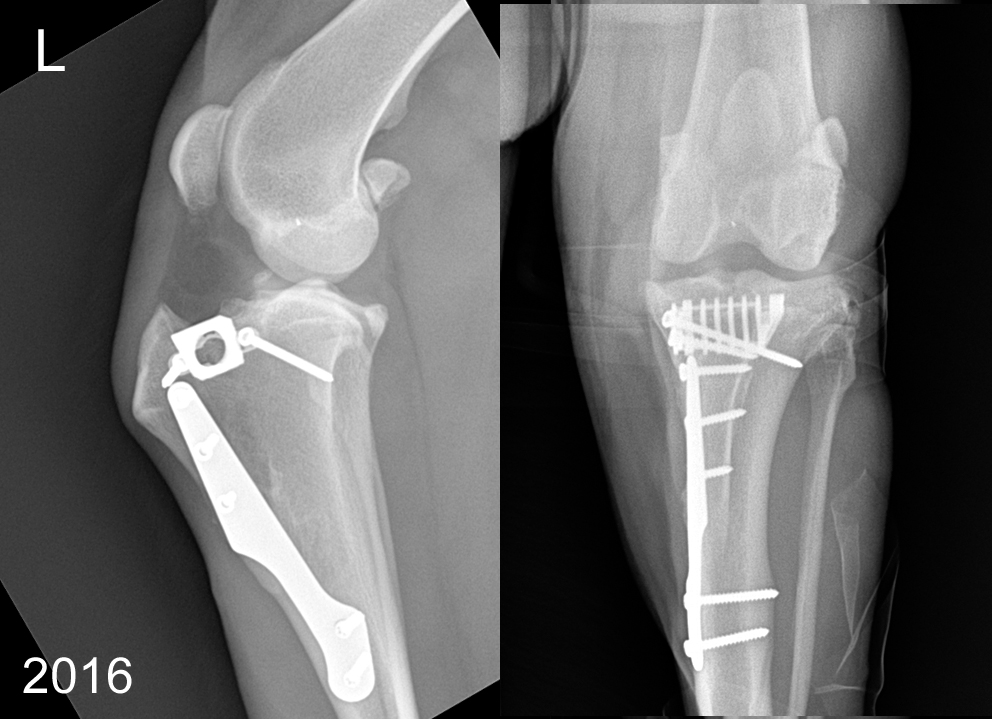
Two years ago, Eri was diagnosed and treated for stifle instability. Then, the clinical signs had started sub acutely and had progressed to moderate persistent lameness, not responding to NSAIDs therapy. The “Drawer” sign was negative, but the cranial tibial compression moderately positive. Stressed X- ray revealed femuro-tibial translation.
A surgical treatment by TTA was applied. The planning of the technique was based on classic method (not the common tangent); fork-less system and 12 mm titanium cage were used. During the procedure mini medial arthrotomy was done and the stifle explored. We found partially torn and fibrillated cranio-medial ligament bundle; the rest of the cranial cruciate looked intact. This part was not debrided (looking strong). Caudal cruciate ligament and both meniscuses were probed and appreciated as normal. Meniscal release was not done.
After the surgery, the dog showed fast clinical improvement with lameness disappearing within 2 weeks post op. A full osteotomy bone healing was confirmed on the 6-th week post op; the activity level was gradually increased to normal. The owner reported an excellent perceived quality.
One year later, Eri was presented to us with similar signs of the opposite, right leg. We found the right knee to suffer from identical pathology: partial cranial cruciate rupture with intact menisci. This time Cora Based Tibial Plateau Leveling Osteotomy (CBLO) was accomplished, again with fast clinical improvement.
Present lameness
In the recent months, Eri became symptomatic on the left leg again. The reported lameness was mild and intermittent, more pronounced after long walks. The owner noticed often weight shift to the right side of the body, when standing. The dog was responding to NSAIDs, but with overall lameness persistence.
Physical examination.
During our examination we found very good athletic body condition. We distinguished intermittent mild (II/V) weight baring lameness and positive sit test on the left side. The musculature of the left leg was obviously weaker than the right one. During ROM testing, Eri was comfortable, but anxiety was elicited during stifle external and internal rotation in moderate flexion (“Mac Murray’s test”). Digital compression of the medial joint capsule was doubtfully appreciated as painful. There was slight decrease flexion ROM; the stifle was found grossly unstable: positive drawer test, but tibial compression test was negative. The patella was stable with maneuvers. Neurological tests were normal.
Barely noticeable left hind leg lameness at the examination, 2016.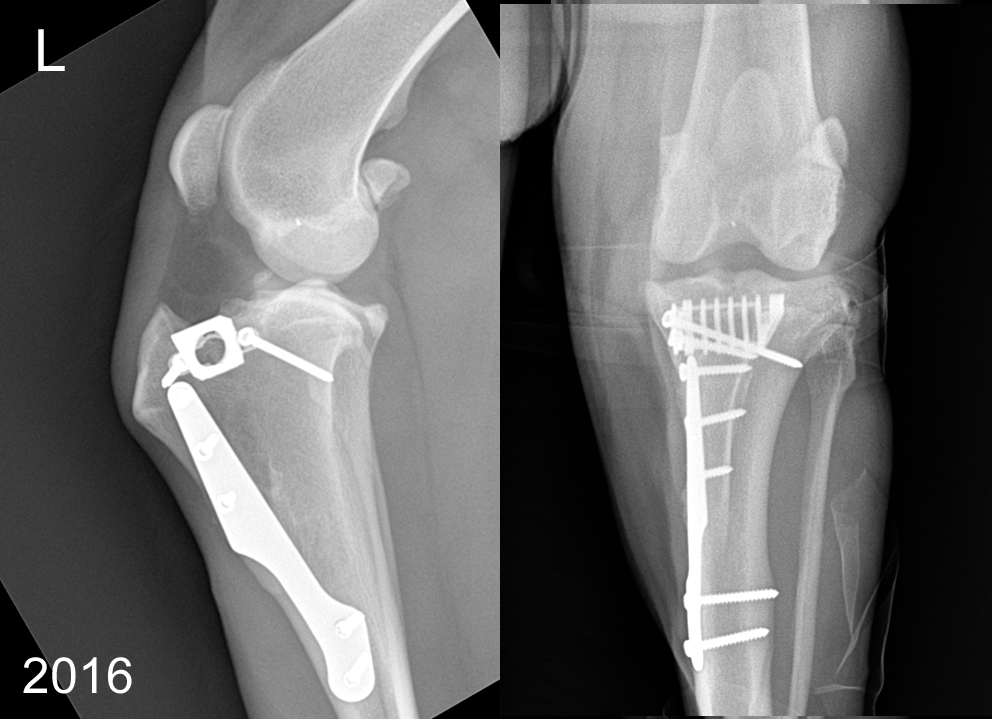
- Orthogonal radiographs were made, revealing:
- normal bony structure
- stable implants
- several small osteophytes present
- mild effusion/capsule thickening
- mild mineralization area just next to extensor fossa
- obviously mineralized structure in the cranial femuro-tibial joint (lateral view)
- cloudy opacifications in the centro-medial and lateral compartment of the joint
Based on the depicted clinical history, clinical signs and X-rays, please make a list of possible differential diagnoses, causing the lameness:
- Late intra-articular septic infection
- Progression to full cranial cruciate ligament rupture
- Rupture /luxation of the long digital extensor
- Suboptimal tuberosity advancement (continuously subluxating knee)
- Meniscus pathology
- Medial collateral instability
- Rupture of the caudal cruciate, caudal tibial thrust
- Patella baja
- Patellar ligament desmitis
- DJD progression
What would be your next diagnostic tests?
- Specific stress X- rays views
- Joint tap
- MRI
- CT
- Stifle arthroscopy
- Exploratory surgery
- Nothing- will recommend physiotherapy
Question yourself!
- What are common long-term clinical consequences after cranial cruciate ruptures?
- What are the chances that TTA prevents them?
- What are the first choice treatments for them, if diagnosed? Can they be managed conservatively?
- Can you build a precise diagnosis based on the clinical exam and radiographs?
Answers:
From the presented information, one should suppose Meniscal Pathology as the most probable cause of the dog’s lameness.
There are number of post op conditions after TTA (or other “geometric osteotomies”) for the unstable stifle. The short term complications could be various: delayed bone healing, implant instability, post operative infection, suboptimal geometric correction, secondary patellar luxation, iatrogenic damage of the medial collateral ligament or long digital extensor muscle, patellar ligament inflammation (desmitis), high or low patella position - patella baja or alta and others. All of the mentioned are typical for the short postoperative period and no radiographic evidence was seen in the presented case.
In long term, there are two most common causes for lameness after cruciate ligament treatment- degenerative joint disease (DJD) progression and late meniscal damage. The cause for these may vary and there are still many controversial aspects, but a residual stifle instability (rotational or other) is supposed to play a major role. Reported statistical incidence of late meniscal damages after TTA is between 7,2% and 14,7 %1,2. This is a higher than the TPLO reported results 1-4,3% 3,4. It has been stated that the meniscal procedure release decreases the chance for late meniscal damage. It should be known that the procedure is again controversial: studies have shown that this interferes with normal stifle biomechanics and may cause faster DJD progression 5.
In Eri’s case, radiograph signs of significant DJD progression were not obvious. This still did not exclude localized focal cartilage damages, but this is difficult to confirm by X-rays. Generally, radiographs do also not diagnose meniscal injuries, but still mineralization changes (like these in the case) could be suggestive. The clinical tests- medial joint palpating and rotational knee maneuvers could be even more informative. In the presented case these clinical tests were positive, causing discomfort.
Nevertheless the short list of possible long-term complication, the precise diagnosis confirmation and treatment plan demanded further diagnostics tests.
A CT study could be sensitive method for detecting chronic DJD, but is much less informative for meniscus and cartilage integrity examination. For the evaluation of the last, the MRI offers better image quality of soft tissues. The MRI is commonly used in human orthopedics for meniscal pathology evaluation.
There are some disadvantages of stifle’s MRI in veterinary medicine- need for general anesthesia, in small patients it could be still difficult to evaluate, need for special imaging skills expertise, no dynamic testing of the meniscal structures (probing), no option for intervention (treatment) during the procedure.
With a possible late meniscal damage, arthrotomy surgery is often the most accessible tool for the veterinary surgeons, yet. There is a diagnostic and therapeutically potential in the procedure. The meniscal visualization could be still inferior in the most challenging cases (small, tight knees). The morbidity with a second joint exploration could be an issue 6. Still in cases with strong suspicion it is highly justified, because of the beneficial effect of an indicated meniscectomy- full or partial.
The arthroscopy offers greatly improved meniscal evaluation (magnified) even in the most caudal joint compartments. The morbidity for the patient is proved to be less with this mini invasive technique 6. With arthroscopy surgery, the treatment techniques are more versatile and precisely applied in a tight joint. The only disadvantages are the equipment high cost and steep learning curve for mastering.
Treatment
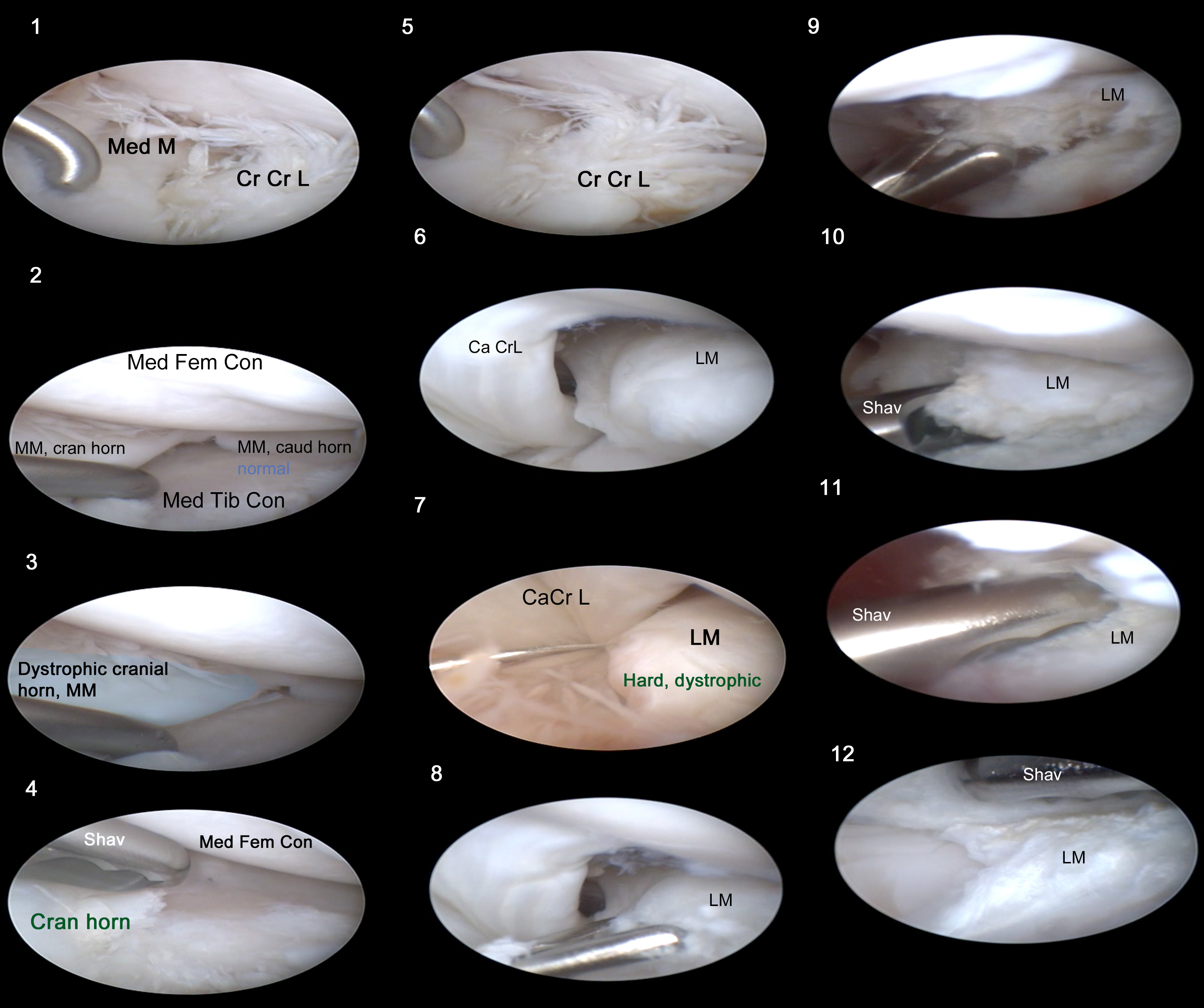
Suggesting, late meniscal damage in Eri’s case, we performed arthroscopic examination, pathology confirmation and treatment. A stifle distractor was used, providing widening the joint space for evaluation. Full set of arthroscopic instruments (including motorised shaver) was prepared, because a need for meniscal intervention was expected. Lateral scope port was used, intermittently changed with medial and again lateral.
What we found in the knee joint was appreciated as un- common meniscal pathology. Along with mild synovitis, we found moderate changed elasticity properties (hardening) of the cranial and central medial meniscus structure with normal caudal horn. A severe hypertrophy and “bone like” appearance of the whole structure of the lateral meniscus was present. Histological study was not done but we supposed a meniscal cartilage dystrophic changes and metaplasia. Possible cause could be chronic abnormal stress to the menisci. Interestingly, in the case, TTA surgery haven’t prevent further cranial cruciate damage- just a small fibrillated bundle was found in the insertion, with the rest part torn and missing. This explains the progression in the “drawer sign” over time- from negative to positive.
Arthroscopy done by Dr. Alexander Chernov, DVM, PhD, Endovet vet center, Kurgan,
<iframe width="560" height="315" src="https://www.youtube.com/embed/T_utiX-lsCw" frameborder="0" allowfullscreen></iframe>
Using a motorised shaver, we were able to perform lateral arthroscopic meniscal reshaping (meniscoplasty). This preserved the lateral meniscal structure. In our understanding this is much more acceptable than the alternative: total lateral meniscal removal, inevitably causing fast consequent fast DJD progression. The procedure for improving meniscal congruity is still palliative, because even reshaped, the meniscus elasticity was suboptimal. We cannot prevent further degenerative progression for sure, but definitely we improved the clinical status of the patient. Eric recovered very well and fast from the procedure- lameness disappeared 7 days later. A close follow up (every 6 months) of the dog and possible intra-articular regenerative therapy is planned in future.
- LAFAVER, S., MILLER, N. A., STUBBS, W. P., TAYLOR, R. A. and BOUDRIEAU, R. J. (2007), Tibial Tuberosity Advancement for Stabilization of the Canine Cranial Cruciate Ligament-Deficient Stifle Joint: Surgical Technique, Early Results, and Complications in 101 Dogs. Veterinary Surgery, 36: 573–586.
- BOUDRIEAU, R. J. (2009), Tibial Plateau Leveling Osteotomy or Tibial Tuberosity Advancement?. Veterinary Surgery, 38: 1–22
- M. S. Bergh, B. Peirone ,IowaState University College of Veterinary Medicine, Ames, Iowa, USA; (2) School of Veterinary Medicine, University of Turin, Turin, Italy, Complications of tibial plateau levelling osteotomy in dogs,Vet Comp Orthop Traumatol. 2012;25(5):349-58
- Gatineau M1, Dupuis J, Planté J, Moreau M..Retrospective study of 476 tibial plateau levelling osteotomy procedures. Rate of subsequent 'pivot shift', meniscal tear and other complications. Vet Comp Orthop Traumatol. 2011;24(5):333-41.
- 5.POZZI, A., KOWALESKI, M. P., APELT, D., MEADOWS, C., ANDREWS, C. M. and JOHNSON, K. A. (2006), Effect of Medial Meniscal Release on Tibial Translation After Tibial Plateau Leveling Osteotomy. Veterinary Surgery, 35: 486–494.
- POZZI, A., HILDRETH, B. E. and RAJALA-SCHULTZ, P. J. (2008), Comparison of Arthroscopy and Arthrotomy for Diagnosis of Medial Meniscal Pathology: An Ex Vivo Study. Veterinary Surgery, 37: 749–755.